Holistic Approaches to Chronic Illness

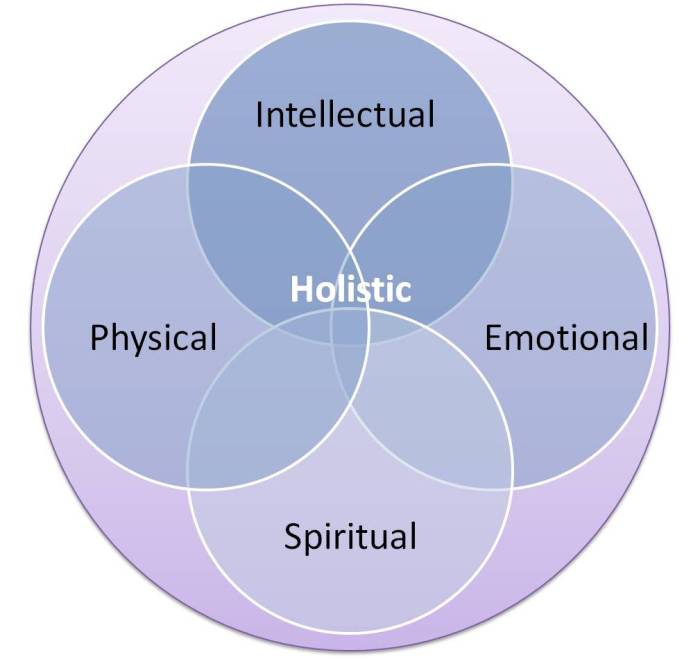
Holistic approaches to chronic illness offer a compelling alternative or complement to conventional medicine. This approach emphasizes the interconnectedness of mind, body, and spirit in managing chronic conditions, moving beyond symptom management to address the root causes of illness. By integrating various therapies like nutrition, stress reduction techniques, and mindfulness practices, holistic healthcare aims to empower individuals to actively participate in their healing journey and improve their overall well-being.
This exploration delves into the core principles of holistic healthcare, contrasting it with conventional approaches. We will examine its application across various chronic illnesses, including diabetes, autoimmune diseases, and chronic pain, highlighting the role of nutrition, the mind-body connection, and effective stress management techniques. Furthermore, we will discuss the importance of mental health support, resilience building, and personal growth in navigating the challenges of chronic illness.
Defining Holistic Approaches to Chronic Illness
Holistic healthcare, in contrast to conventional medicine’s focus on treating specific symptoms or diseases, emphasizes the interconnectedness of mind, body, and spirit in achieving optimal health. When applied to chronic illness management, this approach seeks to address the underlying causes of the condition, not just its manifestations, and to empower individuals to actively participate in their healing journey.
Core Principles of Holistic Healthcare for Chronic Illness
Holistic approaches to chronic illness management are guided by several core principles. These include recognizing the individual’s unique experience of their illness, considering the impact of lifestyle factors (diet, exercise, stress levels, sleep), and integrating various therapeutic modalities to create a personalized treatment plan. The patient is viewed as an active participant in their care, rather than a passive recipient of treatment.
Emphasis is placed on preventative measures and fostering self-healing capabilities. A key element is the collaboration between the patient and healthcare provider to create a shared understanding of the illness and the goals of treatment.
Differences Between Conventional and Holistic Approaches
Conventional medicine typically focuses on diagnosing and treating specific diseases through pharmaceuticals, surgery, or other interventions. It often addresses symptoms directly, aiming for symptom relief and disease management. In contrast, holistic approaches emphasize a broader perspective, investigating the root causes of the illness and considering the individual’s overall well-being. They integrate various therapies to address multiple aspects of the person’s health, aiming for a more comprehensive and sustainable approach to wellness.
While conventional medicine might prescribe medication to manage blood pressure, a holistic approach might incorporate dietary changes, stress reduction techniques, and regular exercise in addition to medication.
Comparison of Holistic Therapies for Chronic Illness Management
Several holistic therapies are used to manage chronic illnesses. These therapies are often complementary to conventional medical treatments, not replacements.
| Therapy | Description | Benefits | Limitations |
|---|---|---|---|
| Acupuncture | Traditional Chinese medicine technique involving thin needles inserted into specific points on the body. | Pain relief, reduced inflammation, improved energy levels. | Not effective for all conditions; may require multiple sessions; potential for bruising or discomfort. |
| Yoga | Mind-body practice combining physical postures, breathing techniques, and meditation. | Improved flexibility, strength, stress reduction, improved mood. | Not suitable for everyone, particularly those with certain physical limitations; requires commitment to practice. |
| Dietary Changes | Modifying food intake to support overall health and manage specific symptoms. | Improved digestion, weight management, reduced inflammation, improved energy levels. | Requires significant lifestyle changes; may be challenging to adhere to; potential for nutrient deficiencies if not carefully planned. |
| Mindfulness Meditation | Practice of focusing on the present moment without judgment. | Reduced stress, improved emotional regulation, increased self-awareness. | Requires consistent practice; may be challenging for some individuals to learn; not a quick fix for chronic illness. |
Benefits and Limitations of Holistic Approaches
The table above provides a brief overview of the benefits and limitations of several holistic therapies. It’s important to remember that the effectiveness of any therapy can vary depending on the individual, the specific condition, and other factors. A holistic approach is not a standalone cure for all chronic illnesses, but rather a complementary approach that can significantly improve the overall well-being and quality of life for many individuals managing chronic conditions.
Careful consideration should be given to the individual’s needs and preferences when selecting therapies, and always consult with healthcare professionals to ensure safe and effective integration with conventional medical treatments.
Holistic Approaches for Specific Chronic Illnesses
Holistic approaches to chronic illness recognize the interconnectedness of mind, body, and spirit in health and disease. Instead of focusing solely on symptom management, these approaches aim to address the underlying causes of illness and promote overall well-being. This section explores the application of holistic methods for managing several common chronic conditions.
Holistic Management of Diabetes
Effective diabetes management requires a multifaceted approach. Lifestyle modifications, including dietary changes and regular exercise, are crucial in regulating blood sugar levels. A holistic approach emphasizes mindful eating, focusing on whole, unprocessed foods, and portion control to maintain stable glucose levels. Regular physical activity, tailored to individual capabilities, helps improve insulin sensitivity and overall metabolic health. Complementary therapies, such as yoga and meditation, can help manage stress, a known factor in blood sugar fluctuations.
These practices aid in promoting relaxation and reducing the physiological responses associated with stress that can negatively impact blood glucose control. For instance, studies have shown that mindfulness-based stress reduction can improve HbA1c levels in individuals with type 2 diabetes.
Holistic Practices in Autoimmune Diseases
Autoimmune diseases, such as rheumatoid arthritis, involve the body’s immune system attacking its own tissues. Holistic practices can play a significant role in mitigating symptoms and improving quality of life. Dietary changes, such as eliminating inflammatory foods and incorporating anti-inflammatory foods rich in omega-3 fatty acids, can reduce inflammation. Stress reduction techniques, including meditation, deep breathing exercises, and yoga, can help regulate the immune system and reduce pain and fatigue.
Other complementary therapies, such as acupuncture and massage therapy, may also provide pain relief and improve overall well-being. For example, a study published in the journal
Arthritis Care & Research* showed that patients with rheumatoid arthritis who participated in a yoga intervention experienced significant improvements in pain, stiffness, and physical function.
Holistic Interventions for Chronic Pain
Chronic pain conditions, like fibromyalgia, can significantly impact a person’s physical and emotional well-being. Holistic interventions aim to address both the physical and psychological aspects of chronic pain. Lifestyle modifications such as regular low-impact exercise, proper sleep hygiene, and stress management techniques are crucial. Complementary therapies like acupuncture, massage therapy, and mind-body practices (e.g., Tai Chi, Qigong) can provide pain relief and improve overall function.
Cognitive behavioral therapy (CBT) can help patients manage their pain by changing negative thought patterns and behaviors. For example, studies have shown that mindfulness-based stress reduction can be effective in reducing pain and improving quality of life in individuals with fibromyalgia.
Holistic Treatment Plans for Chronic Illnesses
| Illness | Lifestyle Modifications | Complementary Therapies | Other Interventions |
|---|---|---|---|
| Diabetes | Balanced diet, regular exercise, stress management | Yoga, meditation, acupuncture | Regular blood glucose monitoring, medication as needed |
| Rheumatoid Arthritis | Anti-inflammatory diet, regular gentle exercise | Acupuncture, massage therapy, yoga | Medication, physical therapy, occupational therapy |
| Fibromyalgia | Regular low-impact exercise, stress management, sleep hygiene | Massage therapy, acupuncture, Tai Chi, Qigong | Cognitive behavioral therapy, medication |
The Role of Nutrition in Holistic Chronic Illness Management: Holistic Approaches To Chronic Illness
Nutrition plays a pivotal role in supporting the body’s natural healing processes and managing chronic illnesses. A balanced diet provides the essential building blocks for repair, strengthens the immune system, and helps regulate bodily functions often disrupted by chronic conditions. Ignoring nutritional needs can significantly hinder recovery and worsen symptoms. A holistic approach emphasizes the profound connection between diet and overall well-being, recognizing food as medicine in the management of chronic diseases.
Dietary Recommendations for Individuals with Chronic Illnesses
Tailoring dietary recommendations to specific chronic illnesses is crucial. For example, individuals with diabetes need to focus on managing blood sugar levels through controlled carbohydrate intake and regular meal timing. Those with heart disease often benefit from a diet low in saturated and trans fats, rich in omega-3 fatty acids, and high in fiber. Individuals with inflammatory conditions may find relief by adopting an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids, while limiting processed foods, sugar, and saturated fats.
Gastrointestinal issues often necessitate dietary adjustments to manage symptoms, such as avoiding trigger foods or incorporating probiotics. Personalized dietary plans, often developed in consultation with a registered dietitian or healthcare professional, are essential for effective management.
Nutritional Deficiencies and Chronic Illness Symptom Exacerbation
Nutritional deficiencies can significantly exacerbate symptoms of chronic illnesses. For instance, iron deficiency anemia can worsen fatigue in individuals with chronic fatigue syndrome, while vitamin D deficiency can exacerbate symptoms of multiple sclerosis. Inadequate intake of essential vitamins and minerals can compromise immune function, impair wound healing, and increase susceptibility to infections – all common challenges for those living with chronic conditions.
Regular blood tests to assess nutrient levels and address any deficiencies are a critical component of holistic chronic illness management.
Nutrient-Rich Foods Beneficial for Managing Chronic Illnesses, Holistic approaches to chronic illness
A balanced diet incorporating a wide variety of nutrient-rich foods is essential. The following list categorizes beneficial foods by nutrient type:
- Antioxidants (Vitamin C, Vitamin E, Beta-carotene): Berries, leafy green vegetables (spinach, kale), citrus fruits, sweet potatoes, nuts, and seeds. These combat oxidative stress, a contributing factor to many chronic diseases.
- Omega-3 Fatty Acids: Fatty fish (salmon, tuna, mackerel), flaxseeds, chia seeds, walnuts. These possess anti-inflammatory properties and support cardiovascular health.
- Fiber: Whole grains (oats, quinoa, brown rice), legumes (beans, lentils), fruits, and vegetables. Fiber promotes healthy digestion, regulates blood sugar, and lowers cholesterol.
- Protein: Lean meats (chicken, fish), legumes, eggs, nuts, and seeds. Protein is essential for tissue repair, immune function, and overall bodily functions.
- B Vitamins: Leafy green vegetables, whole grains, legumes, eggs, meat. B vitamins are crucial for energy production and nerve function.
- Vitamin D: Fatty fish, egg yolks, fortified foods (milk, cereals). Vitamin D plays a crucial role in immune function and bone health.
The Mind-Body Connection in Chronic Illness
Chronic illnesses are rarely solely physical ailments; they are intricately intertwined with the mind and its emotional state. The interplay between physical health and mental well-being is a crucial factor influencing the progression, management, and overall experience of living with a chronic condition. Understanding this mind-body connection is paramount for effective holistic treatment.The impact of stress and anxiety on the progression of chronic illnesses is significant and well-documented.
Prolonged periods of stress trigger the release of cortisol and other stress hormones, which, while beneficial in short bursts, can have detrimental effects on the body when chronically elevated. This constant state of physiological arousal can exacerbate symptoms, impair healing processes, and potentially lead to disease flare-ups or complications. For instance, individuals with autoimmune diseases often experience worsened symptoms during times of high stress, while those with cardiovascular disease may see an increased risk of heart attacks or strokes.
The Impact of Stress on the Immune System
Stress significantly weakens the immune system through various mechanisms. Chronic stress leads to sustained activation of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in prolonged cortisol release. High cortisol levels suppress the activity of lymphocytes, a type of white blood cell crucial for fighting infections and diseases. This immunosuppression increases vulnerability to infections and may hinder the body’s ability to effectively combat existing illnesses, potentially leading to prolonged recovery times or increased susceptibility to complications.
Furthermore, stress can also disrupt the balance of the gut microbiome, further impacting immune function and overall health. The gut microbiome plays a significant role in immune regulation, and stress can alter its composition, potentially contributing to inflammation and immune dysregulation.
Benefits of Stress Reduction Techniques in Chronic Illness Management
Stress reduction techniques, such as meditation and yoga, offer substantial benefits in managing chronic illnesses. These practices help regulate the HPA axis, reducing the production of stress hormones. Meditation, in particular, has been shown to enhance parasympathetic nervous system activity, promoting relaxation and reducing inflammation. Yoga, with its combination of physical postures, breathing exercises, and mindfulness, provides both physical and mental benefits, improving flexibility, strength, and reducing stress levels.
Studies have demonstrated that regular practice of these techniques can lead to improved symptom management, reduced pain perception, better sleep quality, and an enhanced sense of well-being in individuals with various chronic conditions, including fibromyalgia, arthritis, and irritable bowel syndrome.
Incorporating Mindfulness Practices into Daily Routines
Mindfulness practices can be effectively integrated into daily life to improve chronic illness management. A structured approach is beneficial for consistent engagement.
- Start Small: Begin with just 5-10 minutes of daily mindfulness practice. Even short sessions can have a positive impact.
- Choose a Technique: Select a mindfulness technique that suits your preferences and lifestyle. This could be guided meditation apps, body scans, mindful breathing exercises, or simply paying attention to your senses during everyday activities.
- Find a Quiet Space: Create a calm and comfortable environment where you can focus without distractions.
- Focus on Your Breath: Pay attention to the sensation of your breath entering and leaving your body. When your mind wanders, gently redirect your attention back to your breath.
- Be Patient and Kind to Yourself: Mindfulness is a skill that takes time and practice. Don’t get discouraged if your mind wanders; simply acknowledge it and return to your focus.
- Integrate into Daily Life: Practice mindfulness throughout the day by paying attention to your senses during meals, while walking, or engaging in other activities.
- Track Progress: Keep a journal to note your experiences and any changes you observe in your physical and emotional well-being.
Stress and Anxiety Management
Living with a chronic illness often brings significant stress and anxiety. The uncertainty of symptoms, the limitations imposed by the condition, and the ongoing need for medical care can all contribute to a heightened sense of worry and overwhelm. Effective stress and anxiety management is therefore crucial for improving overall well-being and quality of life for individuals facing chronic illness.
This section explores practical coping mechanisms and relaxation techniques to help navigate these challenges.Chronic illness can trigger a cascade of stressful events, from doctor’s appointments and treatment side effects to financial concerns and social isolation. This constant state of heightened alert can exhaust the body’s resources and exacerbate symptoms. Understanding effective coping strategies is vital to break this cycle and promote a sense of control and calm.
Effective Coping Mechanisms for Managing Stress and Anxiety
Developing a personalized approach to stress management is key. This involves identifying personal triggers and developing strategies to address them. Some individuals find journaling helpful to process their emotions, while others benefit from engaging in physical activity or spending time in nature. The goal is to find activities that provide a sense of relief and promote relaxation. It’s also important to remember that seeking support from friends, family, or support groups can significantly reduce feelings of isolation and enhance coping abilities.
Relaxation Techniques to Reduce Stress and Promote Well-being
Relaxation techniques are powerful tools for managing stress and anxiety. These techniques help to calm the nervous system and promote a sense of peace and well-being. Regular practice is key to experiencing their full benefits.
- Deep Breathing Exercises: Focusing on slow, deep breaths can help to slow the heart rate and reduce feelings of anxiety. A simple technique involves inhaling deeply through the nose, holding the breath for a few seconds, and then exhaling slowly through the mouth. This can be practiced anytime, anywhere.
- Progressive Muscle Relaxation: This technique involves systematically tensing and releasing different muscle groups in the body. By focusing on the physical sensations of tension and release, individuals can learn to identify and release muscular tension associated with stress.
- Mindfulness Meditation: Mindfulness involves paying attention to the present moment without judgment. Through meditation practices, individuals can cultivate a sense of awareness and acceptance, which can help to reduce stress and improve emotional regulation. Guided meditations are readily available online or through apps.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing techniques, and meditation to promote relaxation and reduce stress. They can also improve flexibility, strength, and balance.
Resources for Professional Help with Stress and Anxiety
While self-help techniques can be beneficial, seeking professional help is crucial when stress and anxiety become overwhelming or significantly impact daily life. Professional support can provide personalized guidance, coping strategies, and, if necessary, medication management.
- Therapists and Counselors: Mental health professionals can provide therapy, such as cognitive behavioral therapy (CBT) or other evidence-based approaches, to help individuals manage stress, anxiety, and other mental health challenges related to chronic illness.
- Support Groups: Connecting with others who understand the challenges of living with a chronic illness can provide a sense of community and support. Many organizations offer support groups specifically for individuals with particular chronic conditions.
- Doctors and Healthcare Providers: Primary care physicians and specialists can assess the impact of stress and anxiety on overall health and recommend appropriate treatment options, which may include medication, therapy, or a combination of both.
Depression Support Resources
Living with a chronic illness can significantly impact mental well-being, often leading to increased vulnerability to depression and other mental health challenges. Understanding the common mental health struggles experienced by individuals with chronic illnesses and accessing appropriate support systems is crucial for improving their quality of life. This section will explore common mental health challenges, available support resources, and tools for identifying and addressing depression related to chronic illness.
Individuals with chronic illnesses frequently face a range of mental health challenges, with depression being particularly prevalent. The constant pain, limitations in daily activities, and uncertainty surrounding the illness’s progression can contribute to feelings of hopelessness, sadness, and isolation. Anxiety disorders, such as generalized anxiety disorder or panic disorder, are also common, stemming from the worry and stress associated with managing the chronic condition.
Furthermore, chronic illness can exacerbate pre-existing mental health conditions or trigger the onset of new ones. The impact on self-esteem and body image can also be significant, further compounding the mental health burden.
Common Mental Health Challenges in Chronic Illness
The interplay between physical and mental health in chronic illness is complex. Beyond depression and anxiety, individuals may experience other challenges such as:
- Increased irritability and mood swings.
- Difficulty concentrating and impaired cognitive function (“brain fog”).
- Sleep disturbances, including insomnia or excessive sleepiness.
- Social isolation and withdrawal.
- Changes in appetite and weight.
- Feelings of helplessness and loss of control.
Support Systems for Depression Related to Chronic Illness
Fortunately, various support systems are available to help individuals cope with depression related to chronic illness. These resources offer a combination of professional guidance, peer support, and practical strategies for managing both the physical and mental aspects of the condition.
- Therapy: Cognitive Behavioral Therapy (CBT) and other evidence-based therapies can help individuals identify and change negative thought patterns and behaviors contributing to depression. A therapist can also provide coping strategies for managing stress and anxiety related to the chronic illness.
- Support Groups: Connecting with others facing similar challenges can provide a sense of community, shared understanding, and emotional support. Support groups offer a safe space to share experiences, coping strategies, and resources.
- Medical Professionals: Regular communication with physicians, specialists, and other healthcare providers is crucial. They can monitor the patient’s mental health, adjust medication if necessary, and refer them to appropriate mental health professionals.
- Online Resources and Communities: Numerous online platforms and communities offer information, support, and connection for individuals with chronic illnesses and their caregivers. These resources can be particularly helpful for those who may have difficulty accessing in-person support.
Depression Screening Tools and Resources for Seeking Professional Help
Early identification and intervention are crucial in managing depression. Several tools can help assess the presence and severity of depressive symptoms. Seeking professional help is a vital step in receiving appropriate treatment and support.
- Patient Health Questionnaires (PHQ-9): This widely used self-report questionnaire assesses the severity of depressive symptoms over the past two weeks. It helps individuals and healthcare providers gauge the need for further evaluation and treatment.
- Mental Health Professionals: Psychologists, psychiatrists, social workers, and other licensed mental health professionals can provide a comprehensive assessment, diagnosis, and treatment plan for depression. They can offer therapy, medication management, or a combination of both.
- National and Local Resources: Many organizations offer helplines, online resources, and referrals to mental health services. These resources can provide information, support, and guidance in navigating the mental healthcare system.
Mindfulness Practices
Mindfulness, the practice of paying attention to the present moment without judgment, offers a powerful tool for managing the symptoms and emotional challenges associated with chronic illness. By cultivating awareness of bodily sensations, thoughts, and emotions, individuals can develop a greater sense of control and reduce the overwhelming feelings often experienced with ongoing health conditions. This section will explore various mindfulness techniques and their applications in improving self-awareness and emotional regulation for those living with chronic illness.Mindfulness techniques offer a range of approaches to cultivating present moment awareness.
These practices can significantly impact the experience of chronic illness by fostering self-compassion and reducing the intensity of both physical and emotional distress.
Mindfulness Techniques and Applications in Chronic Illness Management
Several mindfulness techniques prove particularly beneficial for managing chronic illness symptoms. Mindful breathing, for example, involves focusing on the sensation of breath entering and leaving the body, anchoring attention to the present and reducing racing thoughts often associated with pain or anxiety. Body scans, a guided meditation where attention is systematically directed to different parts of the body, can increase awareness of physical sensations and help differentiate between pain and other bodily experiences.
Mindful movement, such as yoga or tai chi, combines physical activity with mindful awareness, promoting both physical and mental well-being. Finally, mindful eating involves paying close attention to the taste, texture, and smell of food, fostering a more appreciative and less hurried approach to eating, which can be helpful for those with digestive issues or other conditions impacting appetite and digestion.
Mindfulness and Improved Self-Awareness and Emotional Regulation
Mindfulness cultivates self-awareness by encouraging individuals to observe their thoughts, feelings, and bodily sensations without judgment. This non-judgmental observation allows for a clearer understanding of the interplay between thoughts, emotions, and physical symptoms. By recognizing patterns and triggers, individuals can develop more effective coping strategies. Furthermore, mindfulness enhances emotional regulation by providing a space to acknowledge and accept difficult emotions without getting swept away by them.
This increased emotional awareness empowers individuals to respond to challenges with greater flexibility and resilience, rather than reacting impulsively. For example, a person experiencing chronic pain might notice the onset of anxiety related to their pain and, through mindful observation, develop techniques to manage the anxiety without resorting to unhealthy coping mechanisms.
Guided Meditation for Stress Reduction and Relaxation
Find a comfortable position, either sitting or lying down. Close your eyes gently. Bring your attention to your breath, noticing the natural rhythm of your inhales and exhales. Feel the rise and fall of your chest or abdomen. If your mind wanders, gently guide your attention back to your breath. Now, begin to scan your body, noticing any sensations without judgment. Perhaps you feel tension in your shoulders, or a tightness in your chest. Simply acknowledge these sensations without trying to change them. Imagine a wave of calmness washing over you, gently releasing any tension you may be holding. Continue to focus on your breath, allowing yourself to relax deeper with each exhale. Repeat silently to yourself, “I am safe,” “I am calm,” “I am peaceful.” Continue this practice for 5-10 minutes, or as long as feels comfortable. When you’re ready, gently bring your awareness back to your surroundings, opening your eyes slowly.
Mental Health Advocacy
Living with a chronic illness often presents significant mental health challenges, impacting quality of life and overall well-being. Advocating for improved mental healthcare access is crucial for individuals navigating these complexities. This involves understanding the systemic barriers to care and actively working to remove them.Effective advocacy requires a multi-pronged approach, engaging with both healthcare providers and policymakers to create lasting change.
It’s not simply about receiving better individual care; it’s about building a system that supports the mental health needs of all individuals with chronic illnesses.
Strategies for Effective Advocacy
Engaging in effective advocacy requires a proactive approach. It’s about making your voice heard and working collaboratively with others to create systemic change. This involves understanding the political process and the specific needs of your community.
- Share Personal Stories: Powerful narratives can humanize the issue and resonate deeply with policymakers and healthcare providers. Sharing your personal experience of navigating both chronic illness and mental health challenges can be a compelling way to illustrate the need for better access to care.
- Contact Elected Officials: Reach out to your representatives at the local, state, and national levels. Express your concerns, share your experiences, and advocate for policies that improve mental healthcare access for individuals with chronic illnesses. This can involve writing letters, making phone calls, or attending town hall meetings.
- Collaborate with Healthcare Providers: Work with your healthcare team to identify barriers to mental healthcare access and brainstorm solutions. This collaborative approach can lead to more effective and patient-centered care. For example, advocating for increased mental health screening within chronic illness clinics can lead to early identification and treatment.
- Participate in Public Awareness Campaigns: Join or support organizations that raise awareness about the mental health needs of individuals with chronic illnesses. Spreading awareness is crucial for reducing stigma and increasing public support for improved healthcare access.
The Role of Patient Support Groups and Advocacy Organizations
Patient support groups and advocacy organizations play a vital role in improving mental health outcomes for individuals with chronic illnesses. They provide a platform for sharing experiences, building community, and collectively advocating for change. The collective voice of these groups can be incredibly powerful in influencing policy and practice.
- Community Building and Support: Support groups offer a safe and supportive environment for individuals to connect with others who understand their experiences. Sharing experiences and providing mutual support can significantly improve mental well-being.
- Advocacy and Policy Change: Many organizations actively advocate for policy changes that improve access to mental healthcare. They may lobby policymakers, conduct research, and raise public awareness about the issue.
- Resource Provision: These groups often provide valuable resources, such as information about treatment options, financial assistance programs, and legal aid. This can be especially helpful for individuals facing financial or logistical barriers to care.
- Education and Training: Some organizations offer educational programs and training for healthcare providers, policymakers, and the public about the mental health needs of individuals with chronic illnesses. This helps to improve understanding and reduce stigma.
Therapy and Counseling Options

Living with a chronic illness presents numerous challenges, extending beyond the physical symptoms to encompass significant emotional and psychological impacts. Therapy and counseling offer invaluable support in navigating these complexities, providing individuals with tools and strategies to cope effectively and improve their overall well-being. Different therapeutic approaches cater to various needs, offering personalized support tailored to individual experiences.Therapy can significantly enhance the quality of life for individuals managing chronic illnesses.
It provides a safe and supportive space to process difficult emotions, such as grief, anger, frustration, and fear, often associated with diagnosis, treatment, and ongoing limitations. Furthermore, therapy equips individuals with coping mechanisms to manage pain, fatigue, and other physical symptoms, fostering resilience and promoting a sense of control. Different therapeutic modalities offer unique benefits, addressing specific needs and preferences.
Cognitive Behavioral Therapy (CBT) for Chronic Illness
Cognitive Behavioral Therapy (CBT) focuses on identifying and modifying negative thought patterns and behaviors that contribute to emotional distress. In the context of chronic illness, CBT helps individuals challenge unhelpful thoughts about their condition, such as catastrophizing or focusing solely on limitations. It teaches practical skills for managing symptoms, improving self-efficacy, and promoting adaptive coping strategies. For example, a person experiencing chronic pain might learn to challenge thoughts like “This pain will never go away” and replace them with more realistic and manageable ones, such as “I can manage this pain with the techniques I’ve learned, and it may improve over time.” This shift in perspective can significantly reduce anxiety and improve overall well-being.
Psychotherapy for Chronic Illness Management
Psychotherapy, encompassing various approaches such as psychodynamic therapy and humanistic therapy, offers a broader exploration of the emotional and psychological impact of chronic illness. It delves into the individual’s unique experiences, providing a supportive environment to process complex emotions and gain insight into the relationship between their illness and overall well-being. For instance, exploring past experiences and coping mechanisms can illuminate how an individual responds to their current situation, fostering greater self-awareness and resilience.
This type of therapy can be particularly beneficial for individuals grappling with the existential questions raised by chronic illness.
Finding Qualified Therapists Specializing in Chronic Illness Management
Finding a therapist experienced in working with individuals managing chronic illnesses is crucial for effective treatment. A therapist’s understanding of the specific challenges associated with particular conditions is invaluable.
Here are some resources for finding qualified therapists:
- Your primary care physician or specialist: Often, medical professionals can provide referrals to therapists familiar with chronic illness management.
- Psychology Today’s therapist directory: This online directory allows you to search for therapists based on location, specialization, and insurance.
- The National Alliance on Mental Illness (NAMI): NAMI offers a helpline and resources for finding mental health professionals, including those experienced in working with chronic illnesses.
- Your health insurance provider: Contact your insurance company to obtain a list of in-network therapists who specialize in chronic illness management.
Building Resilience
Living with a chronic illness presents numerous challenges, impacting physical health, emotional well-being, and daily life. Building resilience, however, is crucial for navigating these difficulties and maintaining a fulfilling life. Resilience isn’t about avoiding hardship, but rather about developing the capacity to adapt, cope, and thrive in the face of adversity. It’s about bouncing back from setbacks and finding strength even when things feel overwhelming.Developing resilience involves a multifaceted approach that incorporates practical strategies, emotional regulation techniques, and a commitment to self-care.
By actively engaging in these strategies, individuals can cultivate a stronger sense of self-efficacy and improve their overall quality of life, despite the limitations imposed by their chronic illness. This involves fostering a positive mindset, developing effective coping mechanisms, and building a strong support network.
Strategies for Building Resilience and Coping Skills
Resilience isn’t an innate trait; it’s a skill that can be learned and strengthened over time. Several evidence-based strategies contribute significantly to building resilience in the context of chronic illness. These strategies empower individuals to manage challenges effectively and maintain a sense of control over their lives.
Setting Realistic Goals and Practicing Self-Compassion
Setting realistic, achievable goals is fundamental to building resilience. Instead of striving for perfection, which can be demoralizing, focus on small, manageable steps. Celebrating these small victories reinforces a sense of accomplishment and motivates continued progress. Simultaneously, practicing self-compassion is vital. Acknowledge that setbacks are a normal part of the journey and treat yourself with the same kindness and understanding you would offer a friend facing similar challenges.
Avoid self-criticism and focus on self-acceptance. Remember that progress, not perfection, is the goal.
Activities that Promote Self-Care and Emotional Well-being
Prioritizing self-care is not selfish; it’s essential for building resilience and maintaining overall well-being. Engaging in activities that nurture your physical, emotional, and mental health provides a buffer against the stress and challenges associated with chronic illness.
- Mindfulness and Meditation: Regular mindfulness practices, such as meditation or deep breathing exercises, can help reduce stress, improve focus, and increase self-awareness. Imagine sitting quietly, focusing on your breath, and letting go of anxious thoughts. This cultivates a sense of calm and centeredness.
- Physical Activity: Even gentle exercise, such as walking or yoga, can significantly boost mood, reduce stress, and improve sleep. Visualize yourself taking a leisurely stroll in nature, enjoying the fresh air and sunshine.
- Connecting with Others: Maintaining strong social connections provides crucial emotional support. Picture yourself spending time with loved ones, sharing laughter and conversation. This combats feelings of isolation and loneliness.
- Engaging in Hobbies: Participating in enjoyable activities, whether it’s reading, painting, or gardening, provides a sense of purpose and distraction from the challenges of chronic illness. Imagine yourself immersed in a favorite hobby, feeling a sense of accomplishment and joy.
- Journaling: Expressing thoughts and feelings through writing can be a powerful tool for emotional processing and self-discovery. Visualize yourself writing in a journal, releasing emotions and gaining clarity.
Sleep and Mental Health
Sleep and mental health are intricately linked, particularly for individuals managing chronic illnesses. Sufficient, high-quality sleep is crucial for both physical and mental restoration, and its disruption can significantly exacerbate the challenges posed by chronic conditions. The relationship is bidirectional; chronic illness can disrupt sleep, and poor sleep can worsen the symptoms and overall management of chronic illness.The impact of sleep deprivation on individuals with chronic illnesses is multifaceted and profound.
Lack of sleep directly affects mood regulation, leading to increased irritability, anxiety, and even depression. Energy levels plummet, making it harder to manage daily tasks, participate in therapeutic activities, and adhere to treatment plans. Furthermore, impaired cognitive function, including reduced concentration and memory, hinders self-management strategies and overall quality of life. This cumulative effect creates a vicious cycle, where poor sleep worsens the chronic illness, and the chronic illness further disrupts sleep.
Impact of Sleep Deprivation on Mood, Energy Levels, and Overall Well-being
Sleep deprivation significantly impacts mood regulation in individuals with chronic illnesses. Reduced sleep leads to hormonal imbalances, particularly affecting cortisol (the stress hormone) and melatonin (the sleep hormone). These imbalances can trigger or worsen feelings of anxiety, depression, and irritability. The resulting emotional distress can further complicate the management of the chronic illness itself. Concurrently, energy levels drastically decrease, leading to fatigue and reduced motivation to engage in activities that contribute to overall well-being, such as exercise, social interaction, or adherence to treatment plans.
This lack of energy creates a sense of hopelessness and further exacerbates negative mood states. The cumulative effect of these factors significantly reduces the overall quality of life for individuals living with chronic illnesses. For example, a person with fibromyalgia experiencing sleep deprivation might find their pain levels increase dramatically, impacting their ability to perform even basic daily tasks.
Practical Tips for Improving Sleep Hygiene and Promoting Restful Sleep
Establishing good sleep hygiene is paramount for individuals with chronic illnesses. Consistent sleep schedules, even on weekends, help regulate the body’s natural sleep-wake cycle. Creating a relaxing bedtime routine, such as taking a warm bath or reading a book, signals to the body that it’s time to wind down. Optimizing the sleep environment is also key; this includes ensuring the bedroom is dark, quiet, and cool.
Limiting screen time before bed, as the blue light emitted from electronic devices interferes with melatonin production, is also crucial.
- Maintain a consistent sleep schedule, going to bed and waking up around the same time each day, even on weekends.
- Create a relaxing bedtime routine, such as taking a warm bath, reading a book, or listening to calming music.
- Optimize your sleep environment by ensuring your bedroom is dark, quiet, and cool. Consider using blackout curtains, earplugs, or a white noise machine.
- Limit screen time before bed. The blue light emitted from electronic devices can interfere with melatonin production, making it harder to fall asleep.
- Avoid caffeine and alcohol before bed. These substances can disrupt sleep patterns.
- Get regular exercise, but avoid intense workouts close to bedtime.
- Practice relaxation techniques, such as deep breathing exercises or meditation, to help calm your mind and body before bed.
- If you have trouble sleeping, consider seeking professional help from a doctor or sleep specialist.
Workplace Mental Health
Navigating the complexities of work life while managing a chronic illness presents unique challenges. The workplace, often a source of structure and purpose, can become a significant stressor for individuals facing the physical and emotional demands of chronic conditions. Understanding these challenges and advocating for appropriate support are crucial for maintaining both physical and mental well-being.The impact of chronic illness on workplace performance can manifest in various ways, significantly affecting an individual’s ability to thrive professionally.
Many individuals experience reduced productivity, increased absenteeism, and difficulty concentrating due to pain, fatigue, or emotional distress associated with their condition. These challenges can lead to feelings of inadequacy, isolation, and decreased self-esteem, further exacerbating the impact on their mental health.
Challenges Faced by Individuals with Chronic Illnesses in the Workplace
Individuals with chronic illnesses frequently encounter barriers in the workplace. These obstacles can range from practical difficulties to systemic issues impacting their ability to perform their job effectively and maintain their mental well-being. For example, managing pain or fatigue may require frequent breaks or adjustments to work schedules, which may be met with misunderstanding or resistance from employers or colleagues.
The stigma surrounding mental health also plays a significant role, often leading individuals to conceal their conditions, preventing them from seeking necessary support.
Strategies for Advocating for Workplace Accommodations and Support
Proactive advocacy is key to securing the necessary workplace accommodations and support for individuals managing chronic illnesses. This involves open communication with employers, clear documentation of medical needs, and knowledge of relevant legislation, such as the Americans with Disabilities Act (ADA) in the United States or similar legislation in other countries. A collaborative approach, focusing on finding solutions that benefit both the employee and the employer, is often the most effective strategy.
- Clearly articulate your needs: Provide your employer with a detailed explanation of your condition and how it impacts your work. Use specific examples to illustrate the challenges you face and the types of accommodations that would be helpful.
- Document everything: Maintain a record of all communication with your employer, including emails, letters, and meeting notes. Keep copies of any medical documentation that supports your request for accommodations.
- Explore available resources: Familiarize yourself with relevant workplace policies and legislation regarding disability accommodations. Many organizations offer resources and support for employees with disabilities.
- Consider seeking legal advice: If your employer is unresponsive or uncooperative, consider seeking legal counsel to understand your rights and options.
Importance of Open Communication with Employers Regarding Mental Health Needs
Open and honest communication with employers is crucial for fostering a supportive work environment. This allows employers to understand the challenges employees face and to implement appropriate accommodations and support. It also helps to reduce stigma and create a culture of understanding and empathy within the workplace. The conversation should focus on solutions and collaboration, aiming to find ways to ensure the employee’s well-being while maintaining productivity.
- Choose the right time and place: Schedule a meeting with your employer in a private setting where you can have an open and honest conversation without feeling rushed or pressured.
- Prepare in advance: Gather any relevant documentation and think about what accommodations you need. Be prepared to explain how these accommodations will benefit both you and the company.
- Be assertive but respectful: Clearly state your needs while maintaining a respectful tone. Focus on solutions rather than complaints.
- Follow up in writing: After the meeting, send a follow-up email summarizing the discussion and any agreed-upon accommodations.
Ultimately, managing chronic illness holistically is a journey of self-discovery and empowerment. By embracing a multifaceted approach that addresses the physical, emotional, and spiritual aspects of health, individuals can find sustainable ways to cope with their conditions and enhance their quality of life. The integration of conventional and holistic therapies, coupled with a proactive approach to self-care and mental well-being, offers a path towards improved health outcomes and a greater sense of control over one’s health journey.
This holistic perspective emphasizes the individual’s active participation in their healing, fostering a sense of agency and hope in managing chronic conditions.
Commonly Asked Questions
What are the potential risks of holistic treatments?
Some holistic therapies may interact with conventional medications or have side effects. It’s crucial to discuss all treatments with your doctor, especially if you have pre-existing conditions or are taking medications.
How do I find a qualified holistic practitioner?
Look for practitioners with relevant certifications and experience. Check online directories and seek recommendations from your doctor or trusted sources.
Is holistic treatment covered by insurance?
Insurance coverage for holistic treatments varies widely depending on the specific therapy, your plan, and your location. Check with your insurance provider for details.
Can holistic approaches cure chronic illnesses?
Holistic approaches aim to improve quality of life and manage symptoms, but they don’t always cure chronic illnesses. They are often used in conjunction with conventional medicine.



