Hypertension and Heart Health A Comprehensive Guide
Hypertension and heart health are intrinsically linked, with uncontrolled high blood pressure significantly increasing the risk of serious cardiovascular complications. Understanding the physiological mechanisms behind hypertension, its various risk factors (both modifiable and non-modifiable), and the damaging effects on blood vessels and organs is crucial for effective prevention and management. This guide explores the multifaceted relationship between hypertension and heart health, providing insights into diagnosis, treatment options, and lifestyle modifications that can improve outcomes.
We will delve into the complexities of hypertension, examining its different types, diagnostic methods, and available treatments, including lifestyle changes and medications. Furthermore, we will address the critical role of stress management, mental well-being, and sleep hygiene in mitigating the impact of hypertension. By understanding these interconnected factors, individuals can take proactive steps towards protecting their heart health and improving their overall quality of life.
Hypertension: Hypertension And Heart Health
Hypertension, commonly known as high blood pressure, is a prevalent health concern affecting millions worldwide. It’s a condition where the force of blood against your artery walls is consistently too high, increasing the risk of serious health complications. Understanding its physiological mechanisms and risk factors is crucial for effective prevention and management.
Physiological Mechanisms of Hypertension, Hypertension and heart health
Hypertension arises from an imbalance between the body’s cardiac output (the amount of blood pumped by the heart per minute) and peripheral vascular resistance (the resistance to blood flow in the arteries). Increased cardiac output, often due to factors like increased heart rate or blood volume, can elevate blood pressure. Similarly, increased peripheral vascular resistance, caused by narrowing of blood vessels (vasoconstriction), also contributes significantly.
These factors are often interconnected and influenced by various physiological and lifestyle elements. For example, the renin-angiotensin-aldosterone system (RAAS) plays a key role; when activated, it causes vasoconstriction and sodium and water retention, ultimately increasing blood volume and blood pressure. Additionally, dysfunction in the autonomic nervous system, which regulates blood vessel tone, can also contribute to hypertension.
Risk Factors for Hypertension
Several factors contribute to the development of hypertension, broadly categorized as modifiable and non-modifiable. Addressing modifiable factors is crucial in preventing or managing hypertension.
Modifiable Risk Factors for Hypertension
These are factors that can be changed through lifestyle modifications or medical interventions. Examples include:
- Diet high in sodium: Excessive sodium intake increases blood volume, leading to higher blood pressure.
- Obesity: Excess weight puts extra strain on the cardiovascular system.
- Physical inactivity: Lack of regular exercise weakens the cardiovascular system.
- Excessive alcohol consumption: Alcohol can directly damage blood vessels and increase blood pressure.
- Smoking: Nicotine damages blood vessels and increases heart rate.
- Stress: Chronic stress can elevate blood pressure.
- Diabetes: High blood sugar damages blood vessels and increases the risk of hypertension.
- Sleep apnea: Interrupted breathing during sleep can trigger the release of hormones that raise blood pressure.
Non-Modifiable Risk Factors for Hypertension
These are factors that cannot be changed, including:
- Age: Blood pressure tends to increase with age.
- Family history: A family history of hypertension significantly increases the risk.
- Race: Certain racial groups have a higher prevalence of hypertension.
- Sex: Men tend to develop hypertension earlier than women, but after menopause, the risk increases for women.
- Chronic kidney disease: Kidney dysfunction can disrupt the body’s fluid and electrolyte balance, leading to hypertension.
Types of Hypertension
Hypertension is broadly classified into primary (essential) and secondary hypertension.
Primary Hypertension
This accounts for the vast majority of hypertension cases (over 90%). The cause is often unknown, but it’s believed to be a complex interplay of genetic and environmental factors.
Secondary Hypertension
This type is caused by an underlying medical condition, such as kidney disease, adrenal gland disorders, obstructive sleep apnea, or certain medications. Identifying and treating the underlying condition is crucial in managing secondary hypertension.
Symptoms, Severity, and Complications of Hypertension
Hypertension is often asymptomatic in its early stages. Regular monitoring is essential for early detection.
| Symptoms | Severity | Complications |
|---|---|---|
| Often asymptomatic; may experience headaches, dizziness, shortness of breath, or nosebleeds in severe cases. | Stage 1: 130-139/80-89 mmHg Stage 2: 140/90 mmHg or higher Hypertensive crisis: >180/120 mmHg |
Stroke, heart attack, heart failure, kidney disease, vision loss, cognitive impairment. |
Hypertension and Heart Health
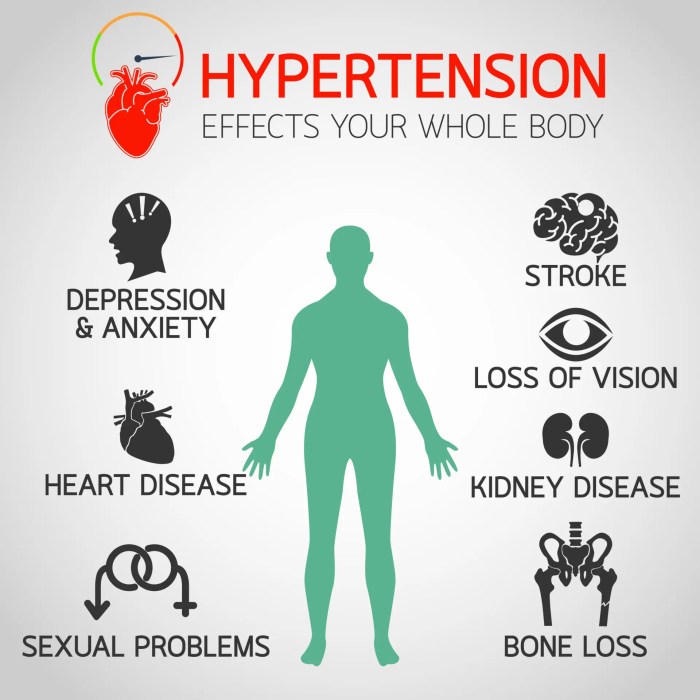
High blood pressure, or hypertension, is a significant risk factor for a range of serious cardiovascular diseases. Understanding the connection between hypertension and heart health is crucial for preventative measures and effective management of this prevalent condition. Ignoring elevated blood pressure can lead to devastating consequences for the heart and circulatory system.Hypertension’s Impact on the Cardiovascular SystemHypertension directly damages blood vessels and organs over time.
The persistent high pressure forces the heart to work harder, weakening its muscle and potentially leading to heart failure. The increased pressure also damages the inner lining of arteries, promoting the buildup of plaque (atherosclerosis), a hallmark of coronary artery disease (CAD). This plaque buildup narrows the arteries, reducing blood flow to the heart muscle, potentially causing angina (chest pain) and eventually a heart attack.
Furthermore, the pressure can weaken blood vessel walls, increasing the risk of aneurysms (bulges in the artery walls) which can rupture and cause internal bleeding. In the brain, hypertension can damage blood vessels, leading to stroke, either through hemorrhagic stroke (bleeding in the brain) or ischemic stroke (blockage of a blood vessel in the brain).Preventative Measures to Mitigate Heart Complications from HypertensionAdopting a healthy lifestyle is paramount in preventing or managing hypertension-related heart complications.
This includes regular physical activity, maintaining a healthy weight, and following a balanced diet low in sodium and saturated fats. Stress management techniques, such as yoga or meditation, can also be beneficial. Regular monitoring of blood pressure is essential, and adhering to prescribed medication, if necessary, is crucial. Quitting smoking, if applicable, is also a vital step, as smoking significantly increases the risk of cardiovascular disease.
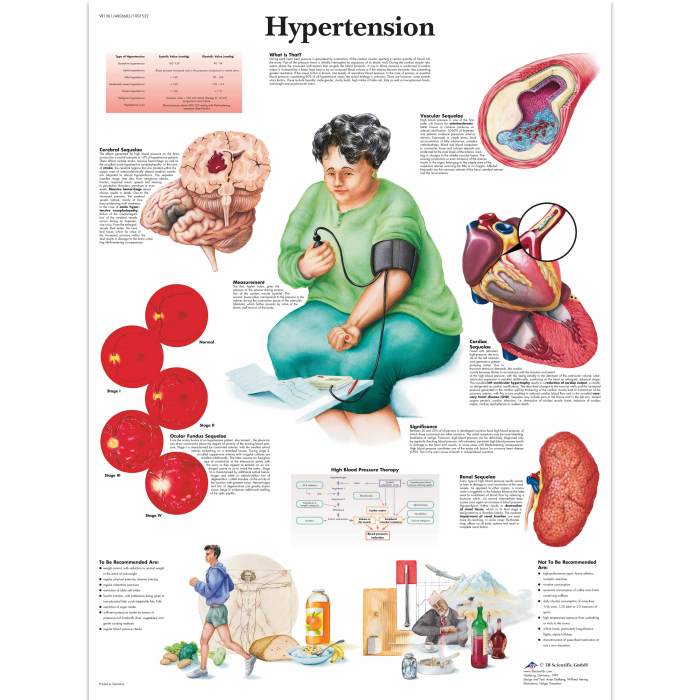
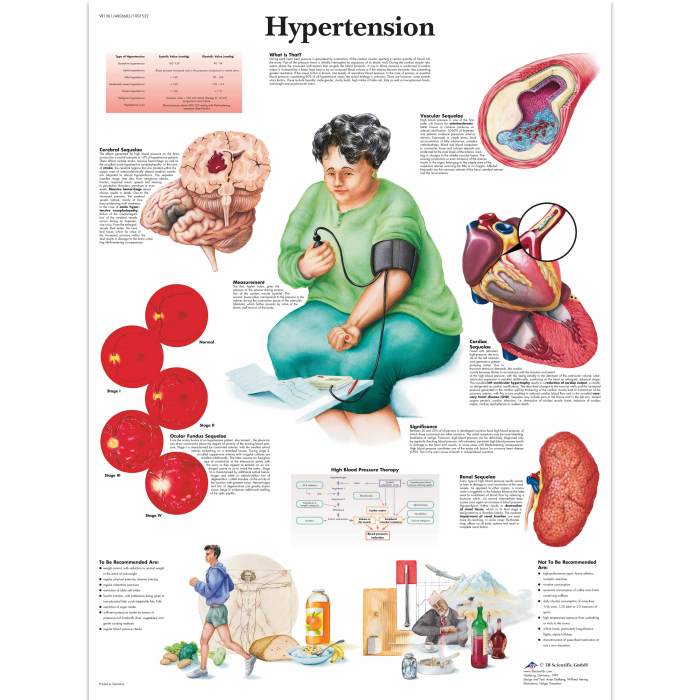
Regular checkups with a healthcare provider allow for early detection and management of hypertension, reducing the risk of long-term complications.Infographic: Hypertension’s Impact on the Cardiovascular SystemThe infographic would visually depict the cardiovascular system, highlighting the effects of hypertension on key areas. The heart would be shown enlarged and strained, symbolizing the increased workload. The arteries would be depicted with narrowed lumens, indicating plaque buildup.
A section would illustrate a weakened artery wall, prone to aneurysm formation. The brain would show a damaged blood vessel, illustrating the risk of stroke. Finally, the infographic would include a healthy cardiovascular system alongside the damaged one, emphasizing the contrast and the importance of preventative measures. The color scheme would use contrasting colors to highlight the areas affected by hypertension, making it easily understandable and impactful.
Stress and Anxiety Management Techniques for Hypertension Patients
Stress and anxiety significantly impact cardiovascular health, and for individuals with hypertension, managing these factors is crucial for overall well-being and blood pressure control. Chronic stress triggers the release of hormones like cortisol and adrenaline, leading to increased heart rate, vasoconstriction (narrowing of blood vessels), and ultimately, elevated blood pressure. This continuous cycle can worsen existing hypertension and increase the risk of heart complications.
Effective stress management strategies are therefore an essential component of hypertension treatment.Stress and anxiety contribute to elevated blood pressure by activating the body’s “fight-or-flight” response. This physiological reaction, while beneficial in acute situations, becomes detrimental when chronically activated due to ongoing stress. The resulting sustained increase in heart rate and vascular resistance directly elevates blood pressure, potentially leading to serious health consequences for hypertensive patients.
Understanding this connection is vital for adopting effective coping mechanisms.
Deep Breathing Exercises and Progressive Muscle Relaxation
Deep breathing exercises, such as diaphragmatic breathing, focus on slow, deep inhalations and exhalations to calm the nervous system. This technique activates the parasympathetic nervous system, counteracting the effects of the sympathetic nervous system (responsible for the “fight-or-flight” response). Progressive muscle relaxation involves systematically tensing and releasing different muscle groups to reduce muscle tension and promote relaxation. Practicing these techniques regularly can significantly reduce stress and lower blood pressure.
For example, practicing diaphragmatic breathing for 10 minutes twice daily can lead to a noticeable decrease in resting heart rate and blood pressure over time. Similarly, consistent progressive muscle relaxation can alleviate muscle tension headaches often associated with stress, indirectly improving blood pressure control.
Mindfulness Practices for Daily Stress Reduction
Mindfulness involves paying attention to the present moment without judgment. Incorporating mindfulness practices into daily life, such as mindful walking, meditation, or mindful eating, can help individuals become more aware of their stress triggers and develop healthier coping mechanisms. Mindful walking, for instance, encourages focusing on the physical sensations of walking—the feeling of the ground beneath the feet, the rhythm of the steps—distracting the mind from anxious thoughts.
Mindful eating promotes awareness of hunger and satiety cues, preventing emotional eating often linked to stress. Regular meditation, even for short periods, has been shown to reduce cortisol levels and improve overall emotional regulation.
Cognitive Behavioral Therapy (CBT) for Hypertension-Related Stress
Cognitive behavioral therapy (CBT) is a type of psychotherapy that helps individuals identify and change negative thought patterns and behaviors that contribute to stress and anxiety. CBT equips patients with tools to manage their stress response, challenge negative self-talk, and develop healthier coping strategies. For example, a CBT therapist might help a hypertensive patient identify situations that trigger anxiety and develop alternative coping strategies, such as deep breathing exercises or positive self-affirmations, to manage these situations effectively.
This approach addresses the root causes of stress and anxiety, leading to more sustainable improvements in blood pressure control and overall well-being. Studies have shown that CBT is effective in reducing blood pressure and improving quality of life in individuals with hypertension.
Depression Support and Resilience Building
Managing hypertension often involves addressing the emotional toll it takes. Depression and hypertension share a complex relationship, with each condition potentially exacerbating the other. Understanding this connection and actively seeking support is crucial for effective management and improved overall well-being.Depression significantly increases the risk of developing hypertension and makes it harder to control existing high blood pressure. The chronic stress associated with managing a chronic illness like hypertension can contribute to depressive symptoms, creating a vicious cycle.
Conversely, untreated depression can lead to unhealthy coping mechanisms, such as poor diet, lack of exercise, and increased alcohol consumption, all of which negatively impact blood pressure. Therefore, addressing depression is not merely a matter of mental health; it’s a vital component of comprehensive hypertension management.
The Relationship Between Depression and Hypertension
Depression and hypertension are frequently co-occurring conditions. The physiological mechanisms linking them involve the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress responses. Chronic stress, often a feature of depression, can lead to sustained activation of the HPA axis, resulting in elevated cortisol levels. Elevated cortisol contributes to increased blood pressure and vascular resistance. Furthermore, depression often leads to lifestyle choices that negatively affect cardiovascular health, such as poor diet, lack of physical activity, and substance abuse.
Seeking professional help is paramount because effective treatment for depression can significantly improve blood pressure control and overall health outcomes.
Depression Support Resources and Helplines
Access to support is vital for individuals dealing with depression alongside hypertension. Several resources are available to provide guidance, counseling, and emotional support.A list of potential resources (note that specific numbers and websites may vary by location; it is crucial to conduct a local search for the most accurate and up-to-date information):
- Your primary care physician: They can provide referrals to mental health professionals and support groups.
- Mental health professionals: Psychiatrists, psychologists, and therapists offer various treatment options, including therapy and medication.
- National helplines: Many countries have national helplines dedicated to mental health support, providing immediate assistance and referrals.
- Online support groups: Online communities offer peer support and a sense of connection for individuals facing similar challenges.
- Support groups for hypertension: Some support groups specifically address the emotional aspects of living with hypertension, providing a safe space for sharing experiences and coping strategies.
Strategies for Building Resilience and Coping Mechanisms
Building resilience involves developing the capacity to bounce back from adversity. For individuals managing hypertension and depression, resilience is crucial for navigating the emotional challenges associated with chronic illness.Strategies for building resilience include:
- Mindfulness and meditation: Practicing mindfulness techniques can help reduce stress and improve emotional regulation.
- Cognitive behavioral therapy (CBT): CBT helps identify and challenge negative thought patterns and develop healthier coping strategies.
- Regular physical activity: Exercise releases endorphins, which have mood-boosting effects and contribute to overall well-being.
- Social connection: Maintaining strong social connections provides emotional support and reduces feelings of isolation.
- Healthy lifestyle choices: A balanced diet, sufficient sleep, and limiting alcohol and caffeine consumption are crucial for both physical and mental health.
Building a Personalized Self-Care Plan
Creating a personalized self-care plan is a proactive step towards managing both hypertension and depression effectively. This plan should incorporate stress management, healthy lifestyle choices, and social support.A step-by-step guide:
- Assess your current situation: Identify your stressors, current coping mechanisms, and areas needing improvement.
- Set realistic goals: Start with small, achievable goals and gradually increase the complexity as you progress.
- Incorporate stress management techniques: Include mindfulness, meditation, deep breathing exercises, or yoga into your daily routine.
- Prioritize healthy lifestyle choices: Focus on a balanced diet, regular exercise, sufficient sleep, and limiting unhealthy habits.
- Seek social support: Connect with friends, family, or support groups to build a strong social network.
- Schedule regular check-ups: Monitor your blood pressure and mental health regularly and consult with healthcare professionals as needed.
- Review and adjust your plan: Regularly review your self-care plan and make adjustments as needed to ensure it remains effective and sustainable.
Sleep Hygiene and Mental Well-being
Sufficient, high-quality sleep is crucial for both mental and physical health, particularly in managing hypertension. Poor sleep significantly impacts cardiovascular health and contributes to stress, anxiety, and depression, all of which can exacerbate hypertension. Understanding the relationship between sleep and blood pressure is vital for effective hypertension management.The impact of poor sleep quality extends beyond daytime fatigue. Chronic sleep deprivation disrupts the body’s natural hormonal balance, leading to increased levels of stress hormones like cortisol.
Elevated cortisol levels contribute to increased blood pressure and can negatively affect the heart’s functioning. Furthermore, inadequate sleep reduces the body’s ability to regulate blood pressure effectively, increasing the risk of cardiovascular events. Conversely, sufficient sleep promotes a healthy cardiovascular system, allowing for better blood pressure regulation and reducing overall stress levels.
The Relationship Between Sleep Disorders and Hypertension
Insomnia, characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep, is strongly linked to hypertension. The chronic stress and physiological changes associated with insomnia contribute to elevated blood pressure. Similarly, sleep apnea, a condition marked by pauses in breathing during sleep, also increases the risk of hypertension. The repeated oxygen drops and sleep disruptions associated with sleep apnea place significant strain on the cardiovascular system, leading to increased blood pressure and an elevated risk of heart disease.
Untreated sleep disorders can significantly worsen hypertension and increase the likelihood of complications.
Recommendations for Improving Sleep Hygiene
Establishing a consistent sleep schedule, even on weekends, is a fundamental step towards better sleep hygiene. This helps regulate the body’s natural sleep-wake cycle, making it easier to fall asleep and wake up feeling refreshed. Creating a relaxing bedtime routine is equally important. This could involve a warm bath, reading a book, listening to calming music, or practicing gentle stretching exercises.
Avoiding caffeine and alcohol before bed is crucial, as these substances can interfere with sleep quality. Optimizing the sleep environment is also essential. This includes ensuring the bedroom is dark, quiet, and cool, and using comfortable bedding.
Practical Steps to Improve Sleep Quality
Prioritizing sleep hygiene involves a multifaceted approach. The following checklist Artikels practical steps individuals can take to improve their sleep quality:
- Maintain a consistent sleep schedule, going to bed and waking up at the same time each day, even on weekends.
- Create a relaxing bedtime routine to signal the body it’s time to sleep. This might include a warm bath, reading, or meditation.
- Optimize your sleep environment by ensuring the bedroom is dark, quiet, and cool. Consider using blackout curtains, earplugs, or a white noise machine.
- Avoid caffeine and alcohol before bed, as these can interfere with sleep.
- Get regular exercise, but avoid intense workouts close to bedtime.
- Make sure your mattress and pillows are comfortable and supportive.
- Create a sleep-conducive atmosphere; this may include adjusting room temperature and minimizing screen time before bed.
- If you are still experiencing sleep problems after trying these steps, consider consulting a doctor or sleep specialist.
Workplace Mental Health and Hypertension
The modern workplace, often characterized by demanding workloads, long hours, and intense competition, significantly impacts employee well-being. Chronic workplace stress is a known contributor to hypertension, a leading cause of cardiovascular disease. Understanding this connection and implementing strategies to mitigate workplace stress is crucial for promoting both employee health and overall organizational productivity. This section explores the link between workplace stress and hypertension, Artikels strategies for improving workplace mental health, and provides guidance for employers on creating a supportive and inclusive work environment.Workplace stress manifests in various ways, leading to a cascade of physiological responses that can elevate blood pressure.
Factors such as job insecurity, heavy workloads, long working hours, lack of control over work tasks, and poor work-life balance can contribute to chronic stress, increasing the risk of developing or exacerbating hypertension. The constant activation of the body’s “fight-or-flight” response, characterized by the release of stress hormones like cortisol and adrenaline, leads to sustained increases in heart rate and blood pressure, ultimately damaging the cardiovascular system over time.
This damage can manifest as hypertension, increasing the risk of heart attack, stroke, and other serious health complications.
Strategies for Promoting Mental Well-being in the Workplace
Promoting mental well-being in the workplace requires a multifaceted approach that addresses both individual and organizational factors. Effective strategies involve a combination of preventative measures, proactive support systems, and a culture shift that prioritizes employee mental health. This includes offering resources and programs designed to reduce stress, improve coping mechanisms, and foster a sense of community and support.
Examples of Workplace Policies Supporting Employee Mental Health
Several workplace policies can demonstrably support employee mental health and well-being. These policies should be clearly communicated and easily accessible to all employees. Examples include flexible work arrangements (allowing for compressed workweeks, telecommuting, or flexible start/end times), generous paid time off policies that include sick leave and mental health days, and readily available employee assistance programs (EAPs) providing confidential counseling and support services.
Furthermore, robust training programs for managers on recognizing and addressing employee stress and mental health concerns are vital. These programs should equip managers with the skills to support employees effectively and create a more empathetic and understanding work environment. Finally, implementing stress management programs, such as mindfulness training or yoga classes, can help employees develop effective coping mechanisms for managing stress.
A Guide for Employers on Fostering a Supportive Work Environment
Creating a supportive and inclusive work environment that prioritizes employee mental health requires a commitment from leadership and a proactive approach to fostering a culture of well-being. This involves establishing clear policies and procedures that support employee mental health, providing accessible resources and support services, and promoting open communication and a culture of psychological safety where employees feel comfortable discussing their mental health concerns without fear of judgment or reprisal.
Regularly assessing employee well-being through surveys and feedback mechanisms can help identify areas for improvement and ensure that initiatives are effective. Leadership should actively model healthy behaviors and promote work-life balance, creating a culture where employees feel valued and supported. Regular communication regarding mental health initiatives and resources will reinforce the employer’s commitment to employee well-being. Investing in employee training programs that focus on stress management and mental health awareness can empower employees to better manage their own well-being and support their colleagues.
Finally, actively promoting a culture of respect, inclusivity, and empathy can significantly improve the overall mental health of the workforce.
Overcoming Addictions and Promoting Personal Growth
Addressing substance abuse is crucial for managing hypertension. Alcohol and tobacco, in particular, significantly impact cardiovascular health, increasing blood pressure and the risk of heart disease. Quitting these substances is a vital step towards better hypertension management and improved overall well-being. This section explores the connection between addiction and hypertension, Artikels available resources, and emphasizes the role of personal growth in holistic health.The relationship between substance abuse and hypertension is multifaceted.
Nicotine in tobacco constricts blood vessels, leading to elevated blood pressure. Excessive alcohol consumption damages the heart and liver, further contributing to hypertension. Moreover, the stress associated with addiction exacerbates existing health conditions, creating a vicious cycle. Addressing addiction, therefore, is paramount for effective hypertension management.
Resources for Addiction Treatment
Many resources are available for individuals struggling with addiction. These include support groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), which offer peer support and guidance. Professional help is also readily accessible through addiction treatment centers, therapists specializing in addiction, and healthcare providers who can prescribe medication to manage withdrawal symptoms and cravings. Many online resources offer information and support, but it’s crucial to seek guidance from qualified professionals for personalized treatment plans.
A combination of therapy, medication, and support groups often proves most effective.
Personal Growth and Self-Care Practices for Hypertension Management
Personal growth and self-care are integral components of effective hypertension management. Engaging in activities that promote mental and emotional well-being can significantly reduce stress, a major contributor to high blood pressure. Self-care practices, such as regular exercise, healthy eating, sufficient sleep, and stress-reduction techniques, work synergistically to improve overall health and blood pressure control. This holistic approach addresses not only the physical aspects of hypertension but also the psychological and emotional factors that often accompany it.
Activities Promoting Personal Growth and Self-Discovery
Several activities can promote personal growth and self-discovery. Mindfulness practices like meditation and yoga can help manage stress and improve emotional regulation. Engaging in hobbies, such as painting, gardening, or playing music, provides a creative outlet and fosters a sense of accomplishment. Spending time in nature, pursuing educational opportunities, or joining social groups can enhance self-esteem and provide a sense of belonging.
Journaling allows for self-reflection and emotional processing, while setting personal goals provides direction and motivation. The key is to find activities that are enjoyable and sustainable, fostering a sense of purpose and fulfillment.
Managing hypertension effectively requires a holistic approach that encompasses lifestyle modifications, medical interventions, and proactive mental health strategies. By addressing the interconnectedness of hypertension, heart health, and overall well-being, individuals can significantly reduce their risk of cardiovascular complications and lead healthier, more fulfilling lives. Remember, early detection and consistent management are key to successful long-term outcomes. This guide serves as a starting point; consult your healthcare provider for personalized advice and treatment plans.
FAQs
What are the long-term effects of untreated hypertension?
Untreated hypertension can lead to serious complications including heart attack, stroke, kidney failure, and blindness.
Can hypertension be cured?
While there’s no cure, hypertension is highly manageable with lifestyle changes and/or medication, often leading to normal blood pressure levels.
Is hypertension hereditary?
A family history of hypertension increases your risk, but lifestyle factors play a significant role regardless of genetics.
How often should I check my blood pressure?
Regular monitoring is crucial. Frequency depends on your risk factors and your doctor’s recommendations, but at least annually for most adults.



